For years, turning 50 was the standard milestone for scheduling your first colonoscopy. It’s not a fun screen, but it can be a lifesaver.
When I turned 50, and I remember it well, I was in the midst of a career transition. I had left the office furniture industry after almost 20 years and was in the process of transitioning to a second career as a fitness professional. It’s something that I had wanted to do for a long time, and the circumstances finally lined up to make the move.
I still remember celebrating my 50th birthday with family and starting my fitness career with Life Time Healthy Way of Life just a few short months later. And while I enjoyed my new job, the first year was challenging and a bit of a cultural shock, as I transitioned from corporate, government, and educational sales to working at a gym.
The last thing on my mind was getting a colonoscopy, even though my dad routinely reminded me that it was time. In fact, I pushed the procedure off until early 2021, when it became somewhat ridiculous for me to delay any longer. I then called my benefits department and obtained a list of gastroenterologists in my area.
For the record, I wasn’t intimidated about the procedure. After knee and especially shoulder surgery, I knew the procedure itself would be a cakewalk. The prep, on the other hand, sucks, especially for an athlete who eats a ton daily just to hold on to my weight. Fasting in any form is one of my least favorite things to do, and when combined with the whole going to the bathroom endlessly for hours, count me out.
That was the mindset that proved to be the stumbling block until I determined that I would never want to do the procedure. In fact, my wanting to had nothing to do with it. It was simply the right thing to do for my long-term health.
So, armed with my list of doctors, I started doing my homework and decided to go with Candice Jantz, M.D. From all her online references, I had a good feeling and scheduled a consultation. I still remember going to meet with her at her office in North Dallas, and we discussed the entire procedure, including my least favorite part, the preparation the day before. I negotiated for all I was worth, and yet, as I walked out of her office, chicken broth and Jell‑O would be my only menu options for the day. Oh boy!
Attempt #1
After that meeting, we scheduled my procedure for late February 2021. Who knew the Dallas–Fort Worth metroplex would be hit with a 100‑year snow and ice storm, which caused my procedure to be canceled. Embarrassingly, I slipped back into fear mode, and it would be another three years before I got up the nerve to reschedule my procedure.
When I called Dr. Jantz’s office, I didn’t need to see her again; however, I scheduled a brief phone consult with her MA, Brenda. We discussed my preparation process, which was essentially the same as before, and then moved forward with booking the actual procedure.
Now, I had heard horror stories over the years from various people, and especially my two dads, about having to drink an enormous amount of some sort of liquid concoction that caused a borderline gag reflex, followed by endless trips to the bathroom. So, I was pleasantly surprised when my prep solution arrived at my doorstep. It was two little bottles that couldn’t have been more than 10–12 oz each.
The instructions were simple: drink the first at noon the day before my procedure, and the second at 3 a.m., just five hours before the big event. Otherwise, I was restricted to Jell‑O, chicken broth, and clear liquids. Not including the obvious challenge of starving all day, I was encouraged by the prospect of having to drink only the two small bottles of prep solution. I thought, How hard can this be?
The only challenge is that the prep solution didn’t work. I called Brenda late in the afternoon of my prep and explained what was going on. She suggested that I take magnesium citrate, which is available at most pharmacies. I was familiar with the product, having used it on a few occasions in the past.
So, I ran down the street to Tom Thumb and chugged it down. We agreed, however, that if my body failed to respond, we would ultimately have to reschedule the procedure. After having starved all day, that was the last thing I wanted; however, that’s precisely what happened. Even after the second bottle of prep solution at 3 a.m., my body didn’t respond any more than under normal daily circumstances.
By 4 a.m., I made the decision to reschedule the procedure and called and left a message at the surgery center, as Brenda had directed me. Within a few days, we scheduled my next attempt on a Saturday in mid‑December. I was relieved that I could undergo the procedure on a Saturday, as I would have my weekend (Sunday and Monday) to recover.
Attempt #2
Given the failure of the first prep solution, Dr. Jantz loaded me up with a completely different protocol that seemed simple enough. I picked up the product from the pharmacy at my favorite store, Costco, and the instructions were very straightforward: add one gallon of water and mix thoroughly with the powder already in the container.
The label stated that it was lightly flavored with lemon, and I was instructed to drink 8 oz every 15 minutes from 3 p.m. to 7 p.m. Thankfully, it mostly tasted like plain water with a hint of lemon. That’s to say it wasn’t bad at all. However, three hours later, I was absolutely sick of that stuff. It was all I could do to finish it off, but I did, mission accomplished.
By late afternoon, amid my drink‑fest, I began to doubt the efficacy of the prep solution. I couldn’t help but think about my experience back in September, and so I called my doctor’s office and spoke with Brenda. She suggested that I add a dose of magnesium citrate or milk of magnesia. I opted for the magnesium citrate and zipped down the street to my local Tom Thumb to pick up a bottle.
Thankfully, things finally started moving after about 7 p.m., and it made for a rough evening. I finally went to bed an hour or so later than usual as my insides seemed to have calmed down, and actually slept until my alarm at 5 a.m. The only challenge was that my prep wasn’t ideal, and while certainly better than the previous attempt in September, I was still very doubtful about the procedure.
I just had this horrible feeling that we would have to reschedule again. Fortunately, my check‑in was only two hours away at 7 a.m., so one way or the other, my ordeal would soon be over. When we arrived, I had some paperwork to complete, and then waited patiently for them to call my name.
When the little nurse called for me, the first thing I told her was about the status of my prep. I further explained what had happened back in September, and she asked, “Do you think you can go now?” I replied, “Well, maybe a little. And then what?” She said, “I will take a look and let Dr. Jantz know.” I was mortified and completely embarrassed. She said not to worry, it was simply what we needed to do to determine whether my screen would be a go.
So I did, and she did, and she said, “I think you’re going to be okay. Let me go talk to Dr. Jantz and tell her, and we’ll decide.” She came back and said, “Dr. Jantz said it’s a go, and not to worry about it. We’re going to make it work.” We proceeded, and the whole thing was over in under an hour.
I remember the anesthesiologist wheeling me into the procedure room and Dr. Jantz coming in to say hello before they put me to sleep. It was totally painless, and then the next thing I knew, I was waking up in recovery. My friend Wendi was dutifully waiting with two 20‑oz coffees, each with protein powder, which I had prepared earlier that morning. My coffee never tasted so good after the events of the previous 24 hours.
Dr. Jantz came in briefly and shared that I had one polyp, which she removed. She said it was not an issue; however, she would have it tested and let me know. She also said that since my prep wasn’t ideal, she wanted to see me back in six months. Are you kidding me? You mean we have to do this again? She wasn’t joking.
With the events of the previous fall behind me, I needed more than six months to mentally prepare for another attempt. I managed to schedule my procedure for the end of my company’s annual insurance renewal period. With two weeks to spare, I scheduled my procedure for Friday, September 19th.
Attempt #3
After my struggles with my first two prep attempts, the third attempt’s prep process was completely different, and I was eager to see how my body responded. Unlike the first two preparations, all the products were standard over‑the‑counter items that can be purchased at any pharmacy.
On the day before my procedure, I was able to have my morning coffee and a small bowl of oatmeal at 7 a.m. After that, it would be Jell‑O and chicken broth for the rest of the day. At 10 a.m., I took four Dulcolax tablets, and at noon, I drank 32 oz of Walmart’s Clear sparkling water with a half bottle of Miralax. I purchased flavorless Miralax, hoping that the taste would be tolerable.
My instructions were to drink 8 oz every 10–15 minutes, and the taste wasn’t bad at all. Afterwards, I just worked quietly at my computer, waiting for the fireworks to begin. And I waited, and I waited. Now you know what I started thinking. Here we go again.
As of about 3:30 p.m., I called Brenda at Dr. Jantz’s office and shared with her what was going on. She told me to go ahead and take the bottle of magnesium citrate that I was supposed to take at 5 p.m. Further, she asked if I could go and get more Miralax to take as soon as possible. I assured her that I would and was thankful for Tom Thumb being only minutes away. At that point, I hoped and prayed that nothing would happen while I was away.
Once I was safe back at home, I downed the extra 32 oz of Clear and Miralax and crossed my fingers that everything would be okay. For the record, I still had another round of Miralax to take at 2 a.m. the next morning, which I was not looking forward to. I struggle enough with my sleep without having to purposely get up at 2 a.m. and drink a quart of rocket fuel.
Finally, around 7 p.m., things began to move. And for the next couple of hours, I did my best to watch TV between trips to the bathroom. Once my tummy seemed to calm down, I took a shower and went to bed. Unfortunately, or fortunately, depending on how you look at it, I still had to go multiple times during the night, until 2 a.m.
When my alarm went off, I bounced out of bed and stumbled into the kitchen, where my last dose of prep was waiting. I knocked it out in about thirty minutes and went back to bed. It prompted numerous more trips to the bathroom leading up to my alarm at 5 a.m.
Wendi actually woke me via text just before my alarm, checking to see how I was feeling. I explained that we were facing December all over again and that I was praying for a good outcome. She picked me up at 6:30 as planned, and our check‑in was scheduled for 7:00. After the required paperwork, I sat quietly waiting for them to call my name.
When the nurse came to get me, I shared with her, just as I had in December, the status of my preparation. And just like in December, she had me “go” so she could determine if I was okay to proceed with the test. Thankfully, she gave me a thumbs‑up, and we moved to get me ready.
“Ashley” did a great job of preparing me for the anesthesiologist. She instructed me to take off all my clothes and place them in a plastic bag. She had put a simple gown and a brand‑new pair of socks on the bed and said she would give me a moment to change. As she closed the curtain behind her, it felt somewhat unnerving to be stripped down to nothing with only a thin veil of a curtain hanging between me and an extra‑busy surgery center.
After a few minutes, she returned with warm blankets and got me all tucked into bed. After establishing the intravenous catheter in my right arm, she left me alone to wait for the anesthesiologist. After about fifteen minutes, he came in to explain what would happen next.
Oddly enough, his name was James, which is my first name, and he wheeled me down to the now‑familiar procedure room. Dr. Jantz came shortly afterwards and went around the bed to check on me. She asked about my prep, and I shared that it was pretty rough and that my body still refused to respond in an ideal fashion. She told me not to worry and that everything would be okay. The next thing I remember was waking up in recovery.
Once my head cleared a bit, I could see Wendi standing in front of me as promised, with two 20‑oz coffees with Life Time’s All‑in‑One Protein powder mixed in. I’ve been mixing protein powder with my morning coffee for over 20 years, and it never tastes better than after going through surgery, or, in this case, a colonoscopy.
Dr. Jantz came in, and she said, “You did fine and actually better than back in December. You had two little polyps, which shouldn’t be an issue. I will have them tested and let you know the results. If you’re clear, you won’t have to come back for three years.” And she said, if I was okay in three years, then she would bump it out to five. However, she’s of the mindset not to go longer than five years, whereas in the past, the standard has been every ten years.
I don’t recall the little guy’s name who helped me in recovery to get my clothes on, and then he walked me down the hall to a bench next to the exit door to wait until Wendi pulled up outside. For those unfamiliar, you always have to have someone take you home, as it would be unsafe to drive after the anesthesia.
Once Wendi parked outside, he walked me out and helped me into her car, and we were off. I was home by 9:30, and oddly enough, as hungry as I was, the first thing I wanted was something to drink. And so I mixed a serving of Life Time’s Tropical Breeze pre‑workout with some cherry‑limeade sparkling water. It was excellent and ideally suited to the circumstances.
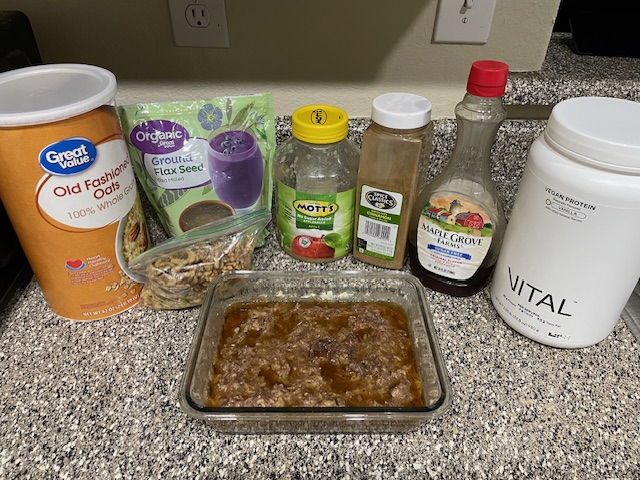
And then it was time for breakfast. My current favorite is oatmeal, but not just any oatmeal. This is Coach Kelly’s Oatmeal, which contains the following:
· Old‑fashioned rolled oats
· Sugar‑free applesauce & cinnamon
· Ground flax seeds & crumbled walnuts
· Cook this mixture in a microwave with water.
Afterwards, stir in a serving of Life Time Vegan Vanilla Protein and then drizzle a little sugar‑free maple syrup on top.
You can enjoy this hot or cold, which reminds me of my pastor, Dr. Jack Graham, whom I have followed for over twenty years. Dr. Graham likes two kinds of pie: hot pie and cold pie. I think that’s hilarious and exactly how I feel about my oatmeal. Either way, it’s excellent.
In all seriousness, the two words that dominated my thoughts upon returning home were relief and gratitude. I was relieved to receive positive feedback from Dr. Jantz and intensely grateful for not having to go through that uniquely challenging experience for three more years.
Why I’m Sharing This
My primary reason for sharing this experience is to educate you if you’ve never undergone the procedure and to encourage you that it’s not as bad as you might think, and is totally worth it. Furthermore, I would like to share a story about one of my close friends and his experience as a cautionary tale, illustrating that a colonoscopy is not something to be avoided or delayed.
Keith Klein was a clinical nutritionist in Houston for over 40 years. I met him in the summer of ’91, right after I graduated from college. I had moved to Houston to start my career, and he has been an influence in my life all these years.
I was a client for the longest time, and then he retired. Shortly afterwards, I started my YouTube channel and reached out to him to come on my podcast. He agreed, and it was during that interview that he shared his journey with colonoscopies with me.
We were discussing longevity and the preventive steps he had taken in his life. Keith is now in his mid‑60s and said that, because of what he had seen in his clinical practice, with more than one patient ending up with colon cancer and/or issues in their 40s, he went through his first colonoscopy at age 45.
Insurance didn’t cover it at the time, but he was happy to pay cash as an investment in his health. The outcome was clear; however, he also decided to undergo the procedure again every five years, rather than the more generally accepted standard of ten years.
His doctor always gave him a bit of a hard time, saying the more frequent screenings weren’t necessary. Keith ignored him and stuck to his guns, opting for screenings at 50 and 55, which turned out great. When he went in for his 60th, his doctor removed a polyp that turned out to be precancerous. If Keith had been on the traditional 10‑year timeline between procedures, that could have ended up in a life‑threatening situation.
I was actually very surprised that I had two polyps in just nine months, because I only had the one the first time. That’s why regular screening is so critical to protect yourself from getting on the wrong side of a cancer diagnosis. I am grateful for Dr. Jantz’s care and look forward to seeing her when I hit the big 60.
Another mentor of my life, Peter Attia, M.D., in Austin, Texas, is a cancer surgeon by training at Johns Hopkins. Today, however, his practice is not based on oncology; it’s about longevity. A cornerstone of his approach to patient care is being a strong advocate for regular screenings, as he views this strategy from the perspective of a cancer surgeon.
He went through his first colonoscopy in his 40s, and his personal rotation is every three years. And in the two odd years, he has used Cologuard. So he’s screening for cancer on an annual basis. And he sums it up like this: there’s no reason for a man to get upside down with either colon or prostate cancer, or a woman with breast or colon cancer, because the screenings are so straightforward.
I didn’t say easy because there’s nothing easy about colonoscopy prep. It sucks, but it’s worth the discomfort. And any of those cancers caught in the early stages are very treatable. But once you go beyond a certain point—once a cancer metastasizes—all bets are off, and the long‑term prognosis is not good.
Final Thoughts
Once I accepted the fact that I would never want to go through a colonoscopy, and that it didn’t matter, it made all the difference in moving forward with the procedure. You do things daily where wanting to has nothing to do with it. You act out of discipline and commitment, and if you apply this same mindset to your health, you will be better off for it.
About ten years ago, I adopted 2 Corinthians 1:3-4 as a life verse, and it provides a framework for how I view life’s struggles. In short, God helps us go through trials so that we can help others navigate similar trials. So, whenever I’m going through a challenging situation, if the only silver lining is that, through my experience, I might be able to help someone in the future going through a similar situation, that’s enough for me.
And it’s in the spirit of 2 Corinthians 1:3-4 that I share this post. The topic is not the most exciting, but it can be a lifesaver. Procrastination is never a good thing in any area of life, especially when it comes to screening for cancer. Forget about whether you want to and simply get it done because it’s the right thing to do for your long‑term health and well‑being.
Best of luck with your journey.













Leave a comment